Introduction: Understanding Rifampicin Biofilm Treatment in Orthopedics
Rifampicin biofilm treatment in orthopedics represents a critical approach to managing one of the most challenging complications in musculoskeletal care. Biofilm-associated infections on orthopedic implants cause persistent, difficult-to-treat infections that conventional antibiotics often cannot eradicate. This comprehensive guide explores the strategic use of rifampicin for biofilm treatment in orthopedic practice, detailing diagnosis protocols, treatment strategies, and preventive measures that can significantly improve patient outcomes.
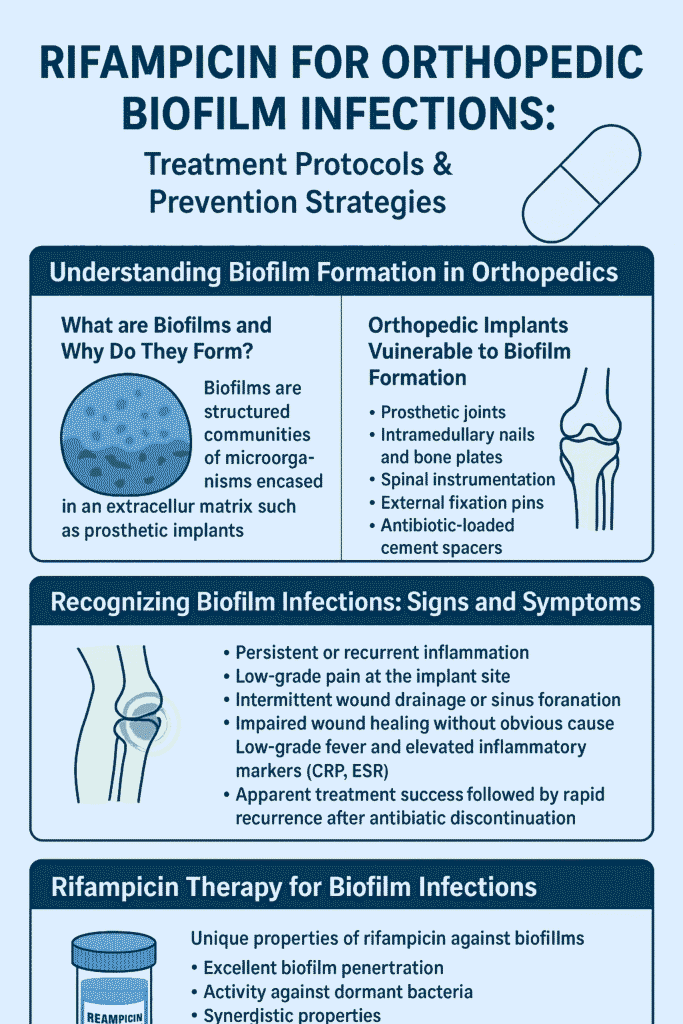
What Are Biofilms and Why Do They Form on Orthopedic Implants?
Biofilms are structured microbial communities encased within a protective extracellular matrix that adhere to biological or inert surfaces. In orthopedic contexts, biofilms form as a defense mechanism when bacteria encounter implant surfaces, where they transition from free-floating cells to organized communities that resist both host defenses and antimicrobial treatments.
The biofilm lifecycle in orthopedics involves:
- Initial attachment of planktonic cells to implant surfaces
- Microcolony formation and extracellular polymeric substance production
- Biofilm maturation with the development of complex structures
- Dispersal of cells to new sites within the joint or implant
Orthopedic Implants Most Vulnerable to Biofilm Formation
Certain orthopedic implants present higher risks for biofilm development:
- Prosthetic joints (hips, knees, shoulders)
- Intramedullary nails and bone plates
- Spinal instrumentation
- External fixation pins
- Antibiotic-loaded cement spacers
The surface characteristics of these implants, including roughness, hydrophobicity, and chemical composition, significantly influence bacterial attachment and biofilm development.
Recognizing Biofilm Infections: Clinical Signs and Symptoms
Indicators of Biofilm-Associated Infections
Biofilm infections often present with subtle signs that differ from acute infections:
- Persistent or recurrent inflammation despite antibiotic therapy
- Low-grade pain at the implant site
- Intermittent wound drainage or sinus formation
- Impaired wound healing without an obvious cause
- Low-grade fever and elevated inflammatory markers (CRP, ESR)
- Apparent treatment success followed by rapid recurrence after antibiotic discontinuation
Diagnostic Challenges in Rifampicin Biofilm Treatment Orthopedics
Traditional diagnostic methods often fail to detect biofilm infections because:
- Standard cultures may yield false negatives due to bacteria existing in a dormant state
- Biofilm bacteria require specialized processing for detection
- Imaging techniques (X-rays, CT scans) may show nonspecific changes
Advanced Diagnostic Approaches for Biofilm Detection
When biofilm infection is suspected, consider these specialized diagnostic techniques:
- Implant sonication: Processing removed implants through sonication to dislodge biofilm bacteria improves culture sensitivity
- Fluorescence imaging: Using specialized light to detect bacterial autofluorescence allows bedside visualization of bacterial loads
- Molecular techniques: PCR and next-generation sequencing can identify pathogens and resistance genes without cultivation
- Histopathological examination: Tissue biopsies revealing microcolonies of bacteria within matrix material confirm biofilm infection
IF you want to reduce Uric Acid in your knee, here we have an article for you containing foods that lower uric acid levels.
Rifampicin Therapy for Orthopedic Biofilm Infections
Unique Properties of Rifampicin Against Biofilms
Rifampicin demonstrates exceptional activity against biofilm-associated infections due to its:
- Excellent biofilm penetration: Ability to diffuse through extracellular polymeric substances
- Activity against dormant bacteria: Effectiveness against stationary-phase and persister cells
- Synergistic properties: Enhanced effectiveness when combined with other antibiotics
When to Initiate Rifampicin Biofilm Treatment in Orthopedics
Initiate rifampicin-containing regimens when:
- Biofilm infection is confirmed or strongly suspected
- Pathogen is susceptible to rifampicin (especially staphylococci)
- Adequate surgical debridement has been performed
- The implant is retained (DAIR procedure – Debridement, Antibiotics, and Implant Retention)
Dosing and Administration Guidelines for Rifampicin Biofilm Treatment
- Loading phase: Begin with standard antimicrobial therapy for 2-7 days before adding rifampicin
- Dosage: 300-450 mg twice daily (or 600-900 mg once daily) for adults with normal liver function
- Timing: Start after initial bacterial burden reduction (typically 3-7 days after other antibiotics)
- Duration: Typically 3-6 months for prosthetic joint infections, depending on clinical response
Combination Therapy Strategies for Optimal Rifampicin Biofilm Treatment
Rifampicin must always be used in combination with other antibiotics to prevent resistance development:
- For methicillin-sensitive S. aureus (MSSA): Combine with β-lactams (flucloxacillin, cefazolin)
- For methicillin-resistant S. aureus (MRSA): Combine with vancomycin, teicoplanin, or daptomycin
- For coagulase-negative staphylococci: Similar approach based on susceptibility profile
Special Considerations for Rifampicin Biofilm Therapy
Monitoring Requirements During Treatment
During rifampicin biofilm treatment orthopedic therapy, regularly monitor:
- Liver function tests (baseline, then every 2-4 weeks)
- Complete blood count (for thrombocytopenia)
- Drug interactions (rifampicin induces cytochrome P450 enzymes)
- Clinical response and signs of toxicity
Managing Drug Interactions in Rifampicin Biofilm Treatment
Rifampicin significantly interacts with many medications, including:
- Anticoagulants (warfarin)
- Cardiovascular drugs (β-blockers, calcium channel blockers)
- Immunosuppressants (cyclosporine, tacrolimus)
- Antidepressants and psychotropic medications
- Oral contraceptives
Dose adjustments or alternative medications may be necessary during rifampicin therapy.
Why not search more about arthritis on our blog inoesis.
Alternative and Adjunctive Biofilm-Targeting Strategies
Complementary Approaches to Rifampicin Biofilm Treatment
While rifampicin remains a cornerstone of biofilm treatment, several adjunctive approaches show promise:
- Quorum-sensing inhibitors: Disrupt bacterial communication pathways essential for biofilm formation
- Enzymatic biofilm disruptors: Dispersion B and DNase enzymes degrade biofilm matrix components
- Metal nanoparticles: Silver, zinc oxide, and other metal nanoparticles demonstrate antibiofilm properties
- Photodynamic therapy: Uses light-activated compounds to produce reactive oxygen species that damage biofilms
Local Delivery Systems for Enhanced Rifampicin Biofilm Treatment
Enhanced local delivery methods improve antibiotic penetration into biofilms:
- Antibiotic-loaded bone cement (PMMA beads or spacers)
- Bioabsorbable antibiotic carriers (calcium sulfate, hydroxyapatite)
- Intrawound antibiotic powder or irrigation solutions
Prevention of Biofilm Infections in Orthopedics
Preoperative Strategies to Avoid Needing Rifampicin Biofilm Treatment
- Patient optimization: Address modifiable risk factors (nutrition, glycemic control, smoking cessation)
- Screening and decolonization: Identify and treat S. aureus carriers with mupirocin and chlorhexidine
- Antibiotic prophylaxis: Administer appropriate antibiotics within 60 minutes before incision
Intraoperative Measures Against Biofilm Formation
- Aseptic technique: Strict adherence to sterilization protocols
- Operating environment: Laminar airflow, limited personnel traffic
- Implant selection: Consider surface-modified implants with antibiofilm properties
- Antiseptic irrigation: Povidone-iodine or chlorhexidine solutions
Postoperative Care to Prevent Biofilm Development
- Early mobilization: Reduces complication rates
- Proper wound care: Maintain sterile dressing changes
- Judicious antibiotic use: Avoid unnecessary antibiotic exposure
We have something special on our website for you to calculate your BMI and weight and have the best strategy to be healthy.
The Future of Biofilm Management in Orthopedics
Emerging technologies and approaches show promise for improving biofilm management:
- Smart implants: Coated with antibiofilm substances or detection capabilities
- Phage therapy: Bacteriophages that specifically target biofilm bacteria
- Immunomodulatory approaches: Enhancing host immune response against biofilms
- Nanotechnology: Advanced delivery systems for biofilm-penetrating antimicrobials
Conclusion: Mastering Rifampicin Biofilm Treatment in Orthopedic Practice
Rifampicin biofilm treatment orthopedics represents a sophisticated approach to managing complex implant-associated infections. The strategic use of rifampicin for biofilm eradication requires careful patient selection, thorough surgical debridement, appropriate combination therapy, and vigilant monitoring for adverse effects and drug interactions.
Successful management of orthopedic biofilm infections demands a multidisciplinary approach involving infectious disease specialists, orthopedic surgeons, microbiologists, and clinical pharmacists. As diagnostic technologies continue to evolve and new therapeutic agents emerge, the prognosis for patients with these challenging infections continues to improve.
By implementing comprehensive prevention strategies, maintaining suspicion for biofilm formation in cases of persistent infection, and applying evidence-based treatment protocols including rifampicin-based regimens, orthopedic practitioners can significantly improve outcomes for patients with device-related infections.
References
- Adjunctive Rifampin Therapy For Diabetic Foot Osteomyelitis
- Controversy about the Role of Rifampin in Biofilm Infections
- Bacterial biofilm formation on implantable devices
- Exploring Reliable Accessible Biofilm Detection Methods
- Evaluation of Antibiotic Resistance and Biofilm Production
- How to recognise wound biofilm
- Therapeutic Strategies against Biofilm Infections
- Antibiotics with antibiofilm activity – rifampicin and beyond
- ESCMID guideline for the diagnosis and treatment of biofilm infections
- Biofilm
Internal Links:
- Understanding Osteomyelitis: A Comprehensive Guide
- Prosthetic Joint Infections: Prevention and Management
- Antibiotic Therapy in Orthopedics: Best Practices
- Wound Care Management for Surgical Sites
External Links:
- CDC Guidelines for Antimicrobial Usage
- Infectious Diseases Society of America (IDSA) Guidelines
- Journal of Bone and Joint Infection
- American Academy of Orthopaedic Surgeons
This article is for informational purposes only and does not constitute medical advice. Consult a qualified healthcare professional for diagnosis and treatment of medical conditions.

Your blog is a breath of fresh air in the often stagnant world of online content. Your thoughtful analysis and insightful commentary never fail to leave a lasting impression. Thank you for sharing your wisdom with us.
thanks for your appreciation.
I do agree with all the ideas you have introduced on your post They are very convincing and will definitely work Still the posts are very short for newbies May just you please prolong them a little from subsequent time Thank you for the post
thanks for your response . can you specifically mention which area should be explained more?
Hello everyone,
I would like to ask for your opinions and experiences regarding website promotion. Nowadays there are so many different options available — SEO, social media marketing, paid ads, influencer collaborations, link building, content marketing, newsletters, etc.
In your experience, which promotional methods are the most effective and efficient in terms of both time and costs? Do some strategies work better for new websites compared to already established ones?
I’d really appreciate hearing your insights, case studies, or even personal tips on what brings the best results in promoting websites.
Thanks in advance!
well thanks for believing in me. The query specifically you asked is interesting and good. and from inductive reasoning i can guess that either you are struggling with a blog or you have started a blog and started promoting it. answer to your question in terms of my personal experience is that . organic SEO is the best thing to do. it takes time. but this is the core of your concern. further it also depends upon your blog or your purpose. like i wanted to build this as my identity in digital world as i wanted to be orthopedic surgeon in future that’s why it was essential for me to make blog like this. also some side hustle like affiliate marketing or content creation or earning by SEO. that’s why i solely was dependent on organic SEO . for you it can be different like if you are selling seasonal product then social media marketing is best. if you are manufacturer then paid promotions and influencer collaboration is best. if you want to be a brand in town or long term permanent business then first SEO, then content marketing, then newsletter and then social media, adds, influencer and link building comes in… . so totally its up to your niche, content type and the purpose of your goals and business. if you can tell me about your intentions i can guide you.
you are in reality a good webmaster The website loading velocity is amazing It sort of feels that youre doing any distinctive trick Also The contents are masterwork you have done a fantastic job in this topic
Your blog is a breath of fresh air in the often mundane world of online content. Your unique perspective and engaging writing style never fail to leave a lasting impression. Thank you for sharing your insights with us.